Knee Osteoarthritis
What is knee osteoarthritis?
There are three kinds of arthritis that can affect the knee: osteoarthritis, inflammatory arthritis, and post-traumatic arthritis. Osteoarthritis (OA) is the most common type of arthritis to affect the knee. Knee OA makes it difficult to perform many daily activities. These include kneeling, climbing stairs, and even walking.
Osteoarthritis affects over fifty million adults in the United States and is the most prevalent musculoskeletal disease. Worldwide, it is estimated that knee osteoarthritis affects 3 percent of the population, or approximately two hundred million people. Osteoarthritis has been reported to account for up to 18 percent of all health care visits and is associated with numerous other health issues, including increased rates of depression and other conditions such as diabetes, obesity, and heart disease. Economically speaking, osteoarthritis is the biggest contributor to work loss each year, costing the US economy roughly $100 billion per year. For comparison, health care costs from osteoarthritis constitute twice the costs devoted to chronic heart and lung disease.
OA is a disease of aging, generally affecting people over the age of 50. OA tends to run in families and women are more often affected than men. Excess weight puts extra pressure on the knee joint, with every pound of weight adding 3-4 pounds of extra weight transmitted across your knees. Additionally, if you are bow legged (misaligned) or put repetitive stresses on the joint, either due to work or athletic endeavors, this can increase the risk of developing OA. Previous traumatic injuries to the knee can also result in post-traumatic OA.
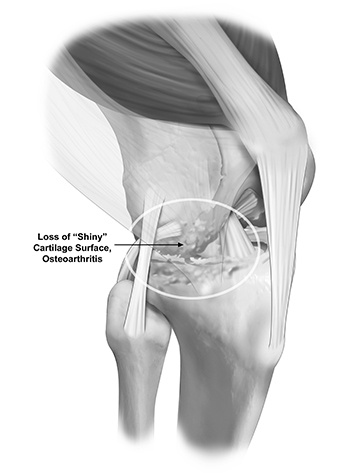
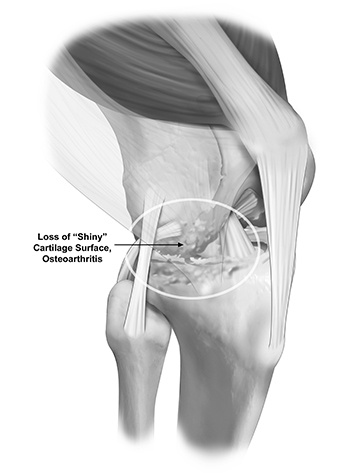
Osteoarthritis (OA) is a chronic, progressive, degenerative disease. It is often called “wear and tear” arthritis because it is the slow deterioration of cartilage, causing the bones to rub against each other. It can affect the shin bone (tibia), the thighbone (femur), and the kneecap (patella).
It is estimated that 85 percent of osteoarthritis originates from changes that are part of the normal aging process (just like gray hairs and wrinkles). The remainder occurs from post-traumatic osteoarthritis (PTOA), which occurs after a knee injury such as an ACL tear or meniscus injury that predisposes the knee to future joint degeneration. It is important to differentiate osteoarthritis (wear and tear changes of the joint) from inflammatory conditions like rheumatoid arthritis, which is an autoimmune disease (where your body attacks its own joints). In autoimmune diseases, the immune system malfunctions and attacks the body instead of intruders. In the case of rheumatoid arthritis, it attacks the synovial membrane that encases and protects the joints, often affecting several joints at one time.
Cartilage does not have nerves and therefore does not cause pain when damaged. However, irritation of the bone beneath the cartilage or the lining of the joint (synovium) that results from cartilage loss can cause pain. Some people have significant OA, but they might not have pain. Common symptoms of knee arthritis include:
- Joint Pain: Knee osteoarthritis typically causes pain in the knee joint. The pain is typically a dull ache felt on either side of the knee or in the front of the knee. The pain often worsens with activity and improves with rest.
- Stiffness: People with knee OA may experience stiffness in the knee joint, making it difficult to move the knee through its full range of motion.
- Reduced Range of Motion: As the condition progresses, the range of motion in the knee joint may become limited, making it challenging to perform activities like walking, bending, or climbing stairs.
- Crepitus: Some people with knee OA may notice a grinding or grating sensation in the knee joint, which is known as crepitus.
- Decreased Function: Knee osteoarthritis can affect a person’s ability to perform daily activities and participate in physical activities.
- Muscle Weakness: The muscles around the knee joint may become weakened due to pain and reduced activity.
- Bone Spurs: Over time, the body may respond to the damage in the joint by forming bony growths or bone spurs at the edges of the joint.
Physical Exam
A comprehensive physical exam will be conducted to assess the range of motion in your knee joint, look for signs of inflammation or swelling, and feel for areas of tenderness or crepitus (grating or grinding sensations). Your gait (the way you walk) will also be evaluated to identify any abnormalities.
Imaging
Diagnostic imaging is necessary to definitively diagnose knee osteoarthritis. X-rays will reveal joint space narrowing, the presence of bone spurs, and the extent of cartilage damage.
Knee osteoarthritis is a degenerative condition that causes joint pain, stiffness, and reduced mobility due to the breakdown of cartilage. As the protective cushioning between bones wears down, daily activities can become increasingly difficult. Leading orthopedic knee surgeon, Dr. Jorge Chahla, specializes in diagnosing and treating knee osteoarthritis, offering personalized care plans designed to relieve pain and improve joint function. If knee discomfort is interfering with your quality of life, Dr. Chahla can help determine the best course of action to manage your symptoms. Schedule an appointment at his office in Chicago, Naperville, or Oak Brook to explore your treatment options.
At a Glance
Dr. Jorge Chahla
- Triple fellowship-trained sports medicine surgeon
- Performs over 800 surgeries per year
- Associate professor of orthopedic surgery at Rush University
- Learn more