Knee Cartilage Injuries Surgical Treatments
What are the surgical options for a cartilage defect?
When nonsurgical treatments do not relieve knee pain or if patients are experiencing catching or locking of the knee joint, then it is reasonable to consider the more definitive treatment option of surgery.
The goal of surgery is to improve symptoms and restore function. In the past decade, there have been significant advancements in the surgical treatment of cartilage defects. Cartilage restoration is one of Dr. Chahla’s areas of expertise and aims at restoring the articular surface in young, active patients.
Surgery for a cartilage defect typically involves a two-stage approach. The first stage includes a diagnostic knee arthroscopy and debridement (chondroplasty) of any loose borders of the focal cartilage defect. If needed, the second stage occurs no earlier than 6-8 weeks following the initial knee scope and involves restoring the cartilage of the focal defect.
A procedure used primarily for symptomatic relief, but also to gather additional information about the focal cartilage defect in the event that future surgery is needed. During this procedure, Dr. Chahla will remove any loose cartilage fragments and smooth the edges of the defect, which decreases friction and irritation. This is usually a good first approach to cartilage injuries because most people will improve with this “minimally invasive” procedure that has almost no downtime. It also allows Dr. Chahla to determine the severity of the injury and plan for any future surgical intervention.
In general terms, a surgeon can choose to use techniques to repair cartilage with procedures that are aimed to “grow” repair tissue over time to cover the cartilage defect. Alternatively, mature cartilage can be transplanted instead and provide immediate coverage of the defect.
Just like with seeding and sodding, the most significant difference is the time it takes to develop a mature grass stand. Sodding is quicker; it’s simply transplanting as cartilage transplants.

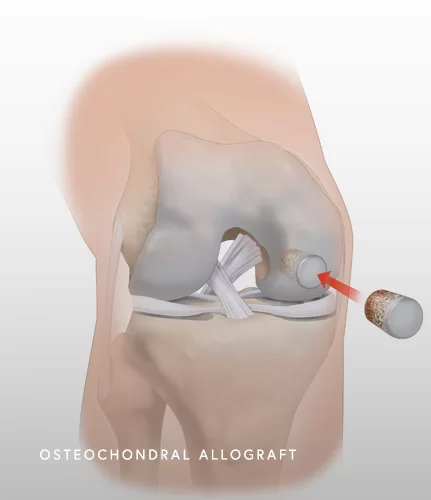
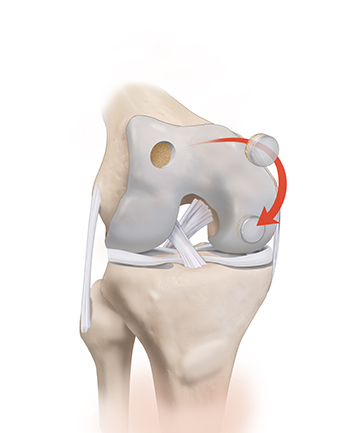
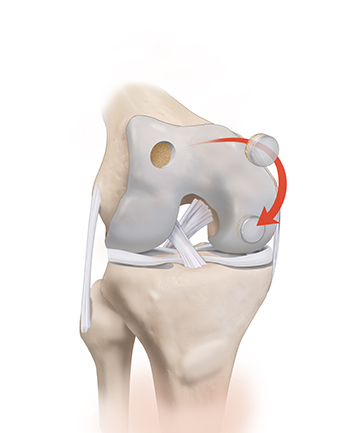
Allografts from a donor (osteochondral allograft) are designed to treat all lesion sizes. This procedure is best for active patients with localized but large defects. These grafts are harvested from a donor and the fresh graft is implanted into the lesion. Survival rates have been reported to be excellent even at 10 years. In most cases of focal cartilage defects requiring surgical intervention beyond the initial diagnostic knee arthroscopy, this is Dr. Chahla’s preferred surgical option.
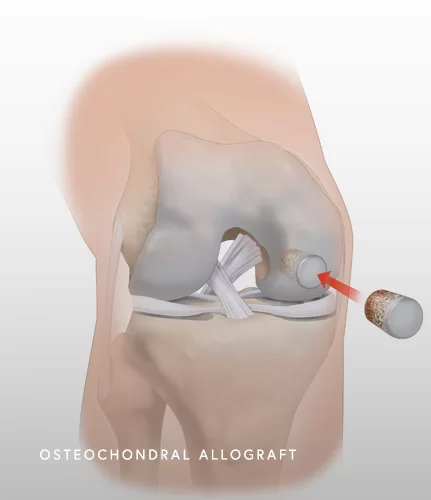
Autografts of cartilage and bone (osteochondral autograft) can also be used to treat these injuries. The cartilage graft is harvested from the patient (autologous) and implanted into the defect. Healthy cartilage is harvested from non-weight bearing portions of the knee joint. This procedure is best for smaller lesions.
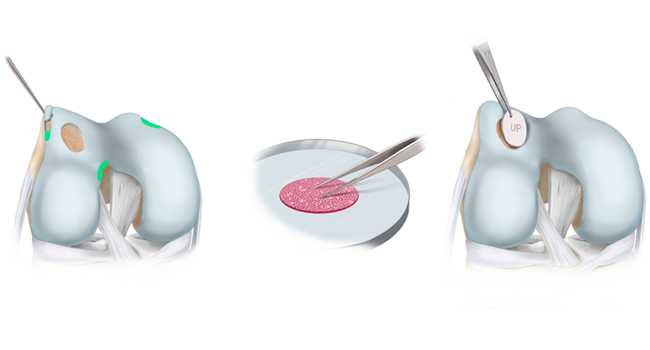
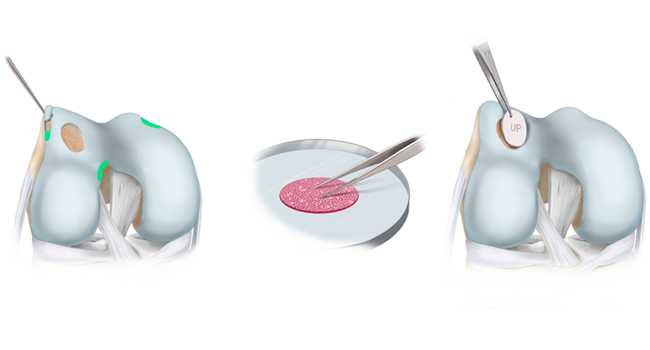
Cartilage transplant or autologous cultured chondrocytes (cartilage cells) on a collagen membrane [MACI] can be used to treat focal cartilage defects. This approach requires two-stages, as it requires an initial arthroscopic procedure to harvest the cells (small biopsy from your cartilage). The patient’s own cartilage cells (chondrocytes) are harvested from a non-weight bearing surface of the knee joint and grown (cultured) in a lab over several weeks. During the initial knee scope, the cartilage lesion is also debrided to remove damaged, unstable cartilage fragments. When ready, the cultured cells are then implanted into a membrane which will then cover the cartilage defect. Because the transplants are made of the patient’s own cells, there is no risk of rejection. MACI is best for younger patients who want to remain active and can commit to post-op rehabilitation. It is most commonly used for patellofemoral (kneecap) cartilage injuries.
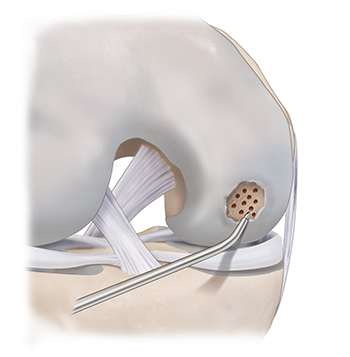
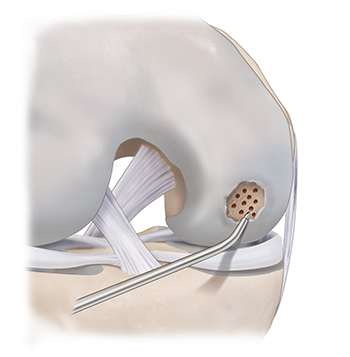
A procedure to create a controlled injury to the bone that will stimulate the bone to create a product similar to cartilage, called fibrocartilage. Fibrocartilage is not as good as articular cartilage but can improve symptoms in certain patients. During a microfracture, tiny holes are made in the bone causing it to bleed, sending bone marrow into the defect to grow new fibrocartilage. Microfracture can be used for patients with limited small cartilage injuries, who are active and desire to return to activity; however, its use has been declining in the last decade.
There are multiple factors that need to be considered to select the best procedure or series of procedures will aid in the best outcome possible. Along with features of the cartilage injury, your goals and activity level should be considered. When treating cartilage defects, every effort should be made to ensure that the cartilage repair area is “protected” and under the best conditions. For this, the alignment of the limb should be corrected if it is abnormal, if there is meniscus insufficiency, a meniscus transplant may be needed and finally if there are any ligament instability it should be addressed concurrently or before the cartilage procedure.
For severe knee cartilage injuries, surgical treatment may be necessary to repair or restore damaged cartilage. Options such as microfracture, cartilage transplant (osteochondral allograft or autograft), and matrix-induced chondrocyte implantation (MACI) can help regenerate cartilage and improve knee function. Dr. Jorge Chahla is a specialist in knee cartilage restoration procedures, utilizing minimally invasive techniques to enhance recovery. If you need surgical intervention for knee cartilage damage, schedule a consultation with Dr. Chahla in Chicago, Naperville, or Oak Brook to discuss your options.
At a Glance
Dr. Jorge Chahla
- Triple fellowship-trained sports medicine surgeon
- Performs over 800 surgeries per year
- Associate professor of orthopedic surgery at Rush University
- Learn more