Meniscus Repair
For most patients with acute traumatic meniscus tears, the best treatment modality is a meniscal repair when indicated. The goal of arthroscopic meniscal repair is to use a minimally invasive surgical technique to bring the torn ends of the meniscus together. These ends are then sutured (stitched) together in an attempt to facilitate healing and restoration of a patient’s natural meniscal contour, shape, and function. This will allow for maximal preservation of a patient’s healthy meniscal tissue and minimize long term damage to the cartilage of the knee. Dr. Chahla believes that a meniscus repair can be considered depending on the state of your cartilage and underlying arthritis, not necessarily on your age. If you are still active, willing to have the repair, and undergo post-operative rehabilitation, you should strongly consider a meniscus repair when indicated.
There are several techniques used for meniscal repair. Like, meniscectomies, the procedure is a minimally invasive arthroscopic surgery that uses small incisions to insert an arthroscope (camera) and arthroscopic tools into the knee joint. Several techniques that are used to bring the meniscal ends together include the all-inside technique, the inside-out technique, the outside-in technique, and the trans-tibial tunnel technique. Each technique has its own respective strengths and weaknesses based on a meniscal tear size/location, and they can be used in combination with each other for larger tears. During the procedure, Dr. Chahla will use the most optimal combination of techniques to achieve the repair that best restores a patient’s native meniscus structure and function.
Dr. Chahla sutures the meniscus without having to make additional incisions. This technique is commonly used for repair of vertical, horizontal, oblique, and some radial tears. Following this repair technique, patients will begin physical therapy the day after surgery, with an emphasis on regaining range of motion and quad activation. Typically, patients are restricted to non-weight bearing for 2 weeks following surgery. However, if the tear was a radial tear, then Dr. Chahla will recommend 6 weeks of non-weight bearing after surgery.

This technique is usually utilized for larger meniscal tears. The inside-out technique places sutures into the meniscus by passing needles from inside the joint to outside the joint. Dr. Chahla will then tie the sutures through an incision on the medial or lateral aspect of the joint depending on the location of the meniscus tear. This technique is considered the gold standard for bucket handle tears because many more sutures can be used, and it can be used to repair complex tears with a high rate of success. The downside of this technique is that it does require an additional incision (which is a small price to pay to save one’s meniscus). Following this repair technique, patients will begin physical therapy the day after surgery, with an emphasis on regaining range of motion and quad activation. Patients will be non-weight bearing for 6 weeks after surgery.
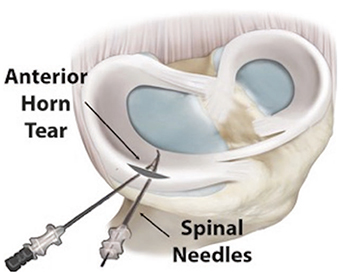
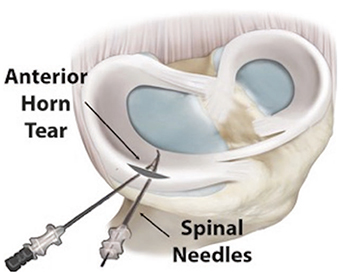
This is a less common technique that involves making a small incision in the front of the knee and passing sutures from outside the knee to inside the knee. This technique is especially important for repairing tears in the front of the meniscus where an inside-out or all-inside meniscus repair technique cannot be used. Following this repair technique, patients will begin physical therapy the day after surgery, with an emphasis on regaining range of motion and quad activation. Patients will be non-weight bearing for 6 weeks after surgery.
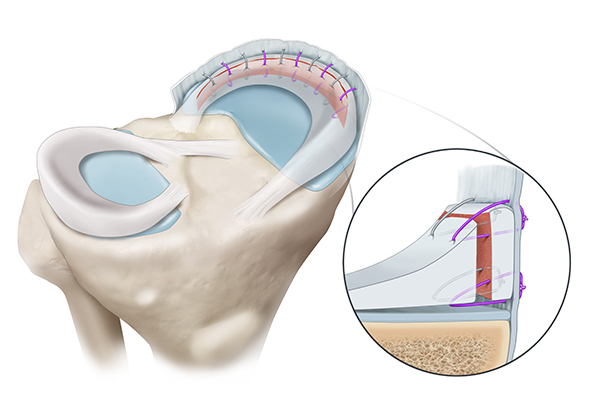
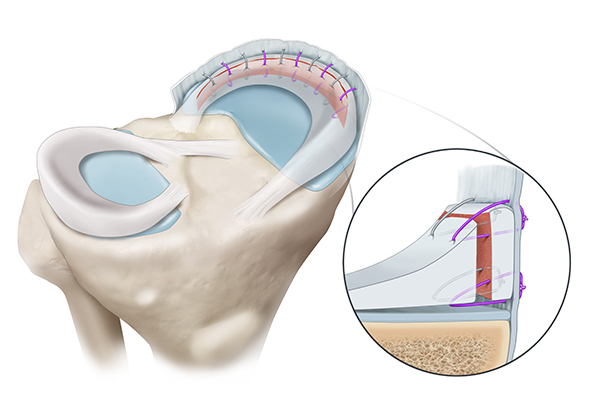
The most common root repair technique is called a transtibial technique. In this technique, sutures are placed into the torn meniscus root and then shuttled down one or two tunnels created in the tibia. Once the meniscus is reduced to its anatomical position, a non-metal anchor is placed in the tibia to hold the tension of the sutures, allowing the meniscus to heal in the correct anatomical location. Following this repair technique, patients will begin physical therapy the day after surgery, with an emphasis on regaining range of motion and quad activation. Patients will be non-weight bearing for 6 weeks after surgery.


Meniscus repair is a surgical procedure aimed at preserving the meniscus by suturing the torn tissue back together. This approach is preferred for certain types of meniscus tears, especially in younger patients or those with tears located in the vascular portion of the meniscus, where healing potential is higher. Leading orthopedic knee surgeon, Dr. Jorge Chahla, specializes in meniscus preservation techniques, utilizing state-of-the-art arthroscopic procedures to optimize healing and long-term knee function. If you have been diagnosed with a meniscus tear and want to explore repair options, contact Dr. Chahla’s office in Chicago, Naperville, or Oak Brook for an expert evaluation.
At a Glance
Dr. Jorge Chahla
- Triple fellowship-trained sports medicine surgeon
- Performs over 800 surgeries per year
- Associate professor of orthopedic surgery at Rush University
- Learn more